
01 May Scientific Progress in Managing Treatment Side Effects for Head and Neck Cancer Survivors
Written by Ron J. Karni, MD
Head and neck cancer patients are experiencing increasing rates of survivorship. This also means many patients are living with the side effects of head and neck cancer treatment. Common side effects I hear from patients include trouble swallowing, voice changes, airway edema (or swelling), neck swelling, muscular scarring, stiffness and decreased range of motion – and none of these are fun. In my practice, we have put great emphasis not just on great cancer treatment, but on improving quality of life during survivorship.
Many of these common side effects can be traced to a condition called lymphedema. Lymphedema can be described as a traffic jam along the highway of lymphatic vessels. Lymphatic vessels exist throughout the body and transport lymph fluid (containing immune molecules and other substances) towards the chest. When cancer infiltrates a lymph node or when a node is removed during surgery, lymphatic flow is interrupted, which can start a cycle of swelling and inflammation.
I wrote an article about lymphedema for SPOHNC back in 2013. At that time, we knew that head and neck lymphedema (HNL) with its associated functional losses affected as many as 75% of head and neck cancer (HNC) survivors 3 months or more after HNC treatment1. However, we didn’t know a lot about why this was happening or how best to treat it. Over the past few years, many physicians including myself conducted studies to understand more. First, how is the treatment of head and neck cancer impacting the onset and progression of lymphedema? Second, what treatments are effective in treating patients’ lymphedema symptoms?
In answering the first question, we conducted trials using infrared imaging to see how lymph fluid moved during various stages of cancer treatment. What we learned was that mild lymphedema may be present before treatment, at the time of head and neck cancer diagnosis.2 Cases of lymphedema increased after radiation therapy; in fact, most patients develop moderate to severe lymphedema after radiation. Early lymphedema causes feelings of tightness, heaviness, or soft swelling, and problems swallowing. Left untreated, tissues become hard and fibrotic which is difficult to treat and it can cause new or worsening symptoms3. Thus, aggressive and early treatment of lymphedema is critical for the best long-term patient outcomes.
This led to our second question: What are effective treatments for lymphedema? A commonly recommended treatment for lymphedema is complete decongestive therapy by a therapist including patient education, manual lymphatic drainage, compression garments, exercise, and skin care. Most HNC patients undergo brief professional therapy followed by a lifetime of daily home self-care. While this approach may prove effective for some patients, lymphedema fails to respond adequately in others4-8. Many other patients experience barriers to access this lymphedema care in the first place including cost or insurance obstacles, lack of certified and experienced lymphedema therapists nearby, and self-limitations (e.g., physical or cognitive impairments). Thus, cost effective, home based treatment options for both primary and refractory lymphedema remains an unmet need.
Although widely used for breast cancer patients with lymphedema, a self-treatment tool that hadn’t yet been studied extensively in head and neck patients was an advanced pneumatic compression device (APCD). An APCD includes an electric air pump and a garment that attaches to it via simple air hoses. The pump inflates the garment providing a gentle, directional massage similar to what a therapist would perform or teach a patient to perform at home. An APCD automates this therapy for more consistent results, making it easy to use for daily home management of symptoms.
In the case of the head and neck, the APCD has two garment pieces; one that fits over the head and another worn as a vest. The vest garment chambers inflate in the chest area first, moving the lymph fluid and creating a pathway for the fluid in the head/neck to move to. Secondly, the head garment chambers inflate and push the lymph fluid downward into the chest.
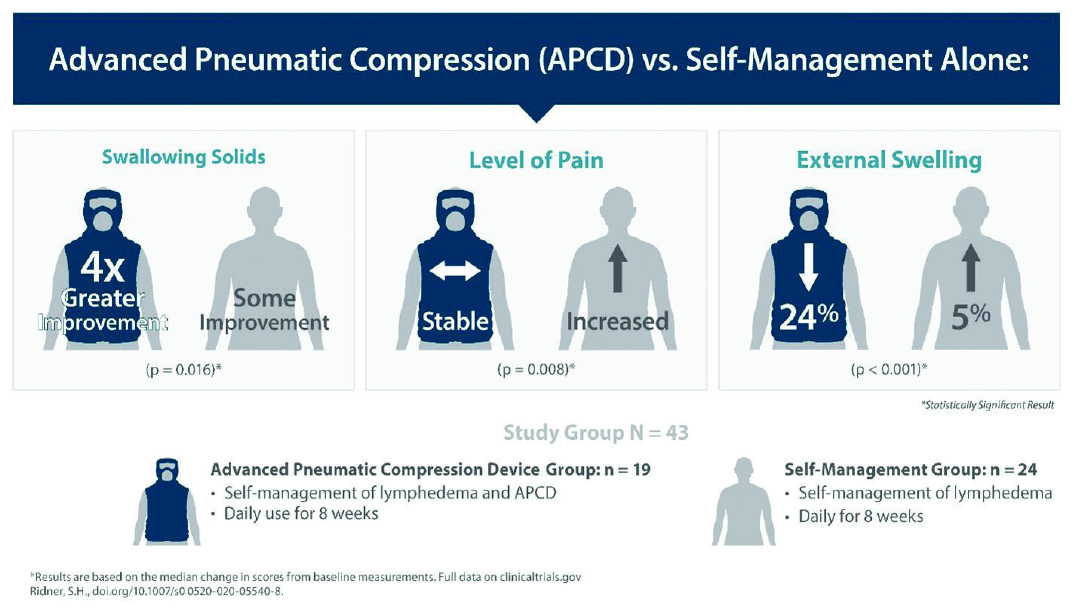
A team of clinicians at Vanderbilt University conducted a study of 43 patients to determine how typical home management would compare to an APCD9. Patients were randomized to either the “usual care” group or the “APCD group.” The patients’ symptoms were measured via clinically validated patient surveys and objective measurements before and after their respective treatments. The results showed statistically significant improvements in symptoms for the patients that used APCD. The most impactful improvements were shown in swallowing solids, reduction in swelling, and stabilized level of pain. Additional improvements were found in mucous related symptoms, the severity of soft tissue related symptoms, and neurological symptoms. This study was published in May of 2020 in the Journal for Supportive Care in Cancer.
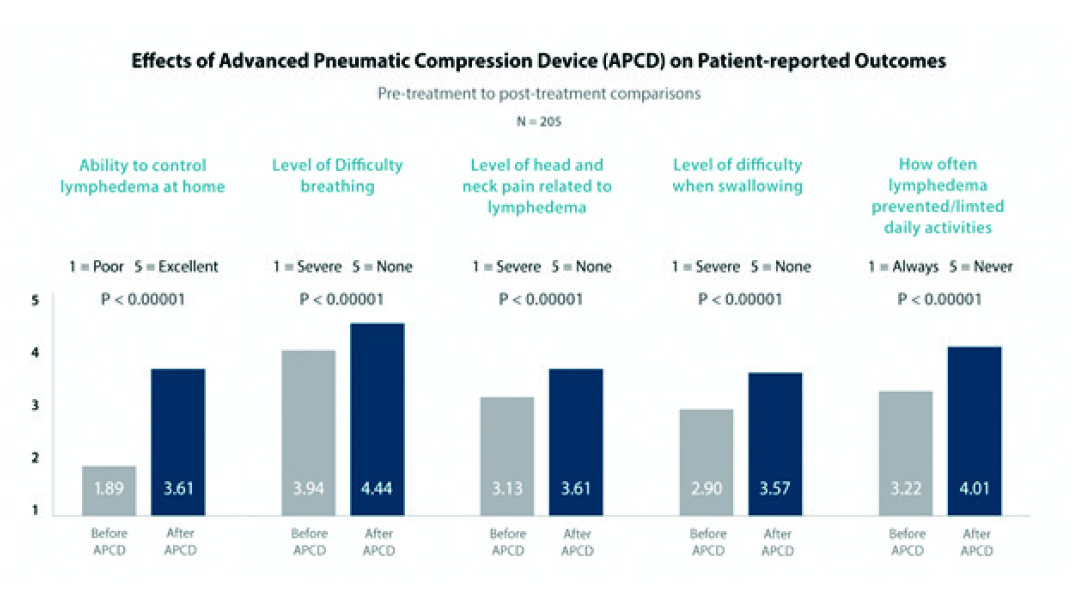
The results described in the 43 patient Vanderbilt study were also seen in a study of a much larger group of 205 patients. A colleague of mine, Dr. Carolina Gutierrez, analyzed the patients’ reported symptoms from before and after they received their Advanced Pneumatic Compression Device. The patients reported on 5 symptoms: 1) Ability to control lymphedema at home, 2) Level of difficulty breathing, 3) Level of head and neck pain related to lymphedema, 4) Level of difficulty when swallowing, and 5) How often lymphedema prevented/limited them from their daily activities. In each of these questions, patients had statistically significant improvements after they used the APCD for 90 days than before they had received it. This study was published in March 2020 in the Journal of the Sciences and Specialties of the Head and Neck.
On the surgery side of things, I am continuing to research and learn how best to minimize the effects of cancer treatment while still completely removing the cancer. On the survivorship side, we continue to work on how best to treat the patients’ symptoms. Research from Dr. Sheila Ridner shows that 90% of head and neck cancer survivors will suffer from lymphedema 1 year out from their treatment1. New therapies like pneumatic compression for self-management can be very impactful for survivor quality of life, especially today when COVID-19 adds to existing access barriers to professional therapy. If you are suffering from the symptoms of lymphedema, tell your doctor. The earlier you receive treatment the better off you will be.
Patient Experience Report:
- Ridner, S.H., et al., A prospective Study of the Lymphedema and Fibrosis Continuum in Patients with Head and Neck Cancer. Lymphat Res Biol, 2016. 14(4): p. 198-205
- Ridner SH, Dietrich MS, Niermann K, Cmelak A, Mannion K, Murphy B (2016) A prospective study of the lymphedema and fibrosis continuum in patients with head and neck cancer. Lymphat Res Biol 14(4):198–205. https://doi.org/10.1089/lrb.2016.0001
- Ridner SH, Dietrich MS, Sonis ST, Murphy B (2018) Biomarkers associated with lymphedema and fibrosis in patients with Cancer of the head and neck. Lymphat Res Biol 16:516–524. https://doi.org/10.1089/lrb.2017.0074
- Yao T, Beadle B, Holsinger CF, Starmer HM (2020) Effectiveness of a home-based head and neck lymphedema management program: a pilot study. Laryngoscope. https://doi.org/10.1002/lary.28549
- Tyker A, Franco J, Massa ST, Desai SC, Walen SG (2019) Treatment for lymphedema following head and neck cancer therapy: a systematic review. Am J Otolaryngol 40(5):761–769. https://doi.org/10.1016/j.amjoto.2019.05.024
- Doke KN, Bowman L, Shnayder Y, Shen X, TenNapel M, Thomas SM, Neupane P, Yeh HW, Lominska CE (2018) Quantitative clinical outcomes of therapy for head and neck lymphedema. Adv Radiation Oncology 3(3):366–371. https://doi.org/10.1016/j.adro.2018.04.007
- Deng J, Sinard RJ, Murphy B (2019) Patient experience of head and neck lymphedema therapy: a qualitative study. Support Care Cancer 27(5):1811–1823. https://doi.org/10.1007/s00520-018-4428-2
- Smith BG, Hutcheson KA, Little LG, Skoracki RJ, Rosenthal DI, Lai SY, Lewin JS (2015) Lymphedema outcomes in patients with head and neck cancer. Otolaryngol Head Neck Surg 152(2):284–291. https://doi.org/10.1177/0194599814558402
- Ridner, S.H., Dietrich, M.S., Deng, J. et al. Advanced pneumatic compression for treatment of lymphedema of the head and neck: a randomized wait-list controlled trial. Support Care Cancer (2020). https://doi.org/10.1007/s00520-020-05540-8
Editors Note: Ron J. Karni, MD serves as Chief of the Division of Head and Neck Surgical Oncology in the Department of Otorhinolaryngology–Head & Neck Surgery at UT Health. He obtained his medical degree at Baylor College of Medicine and then completed his residency training at Washington University in St. Louis School of Medicine. Dr. Karni has authored publications on the novel treatment of occult primary oropharyngeal cancer (the unknown primary) and practical tools to integrate evidence-based methods into the daily practice of medicine. His current research focus includes de-escalation treatment strategies for throat cancer, morphoproteomic analysis of head and neck cancer, and HPV-related malignancies of the head and neck. He is also co-Principal Investigator on a CPRIT grant studying new treatments for head and neck lymphedema using near infrared fluorescent technology. Dr. Karni is board certified by the American Board of Otolaryngology–Head & Neck Surgery.
